How to Boost Your Immune System During Marathon Training
By Lizzie Gralton
Finding Your Balance Dietetics
April 2025
Association Between Exercise and Immune Health
Recent research shows a clear link between the intensity and duration of exercise and the strength of the immune system. In simple terms, there appears to be a “sweet spot” when it comes to training. This idea is often illustrated by the J-Curve (see Figure 1), which suggests that moderate exercise can boost immune function, while excessive training without enough recovery can weaken it.
Other factors like diet and sleep hygiene also play an important role in immune health. However, it's clear that athletes—especially endurance athletes like marathon runners—who train too hard without proper rest or nutrition are at a higher risk of illness and infection.
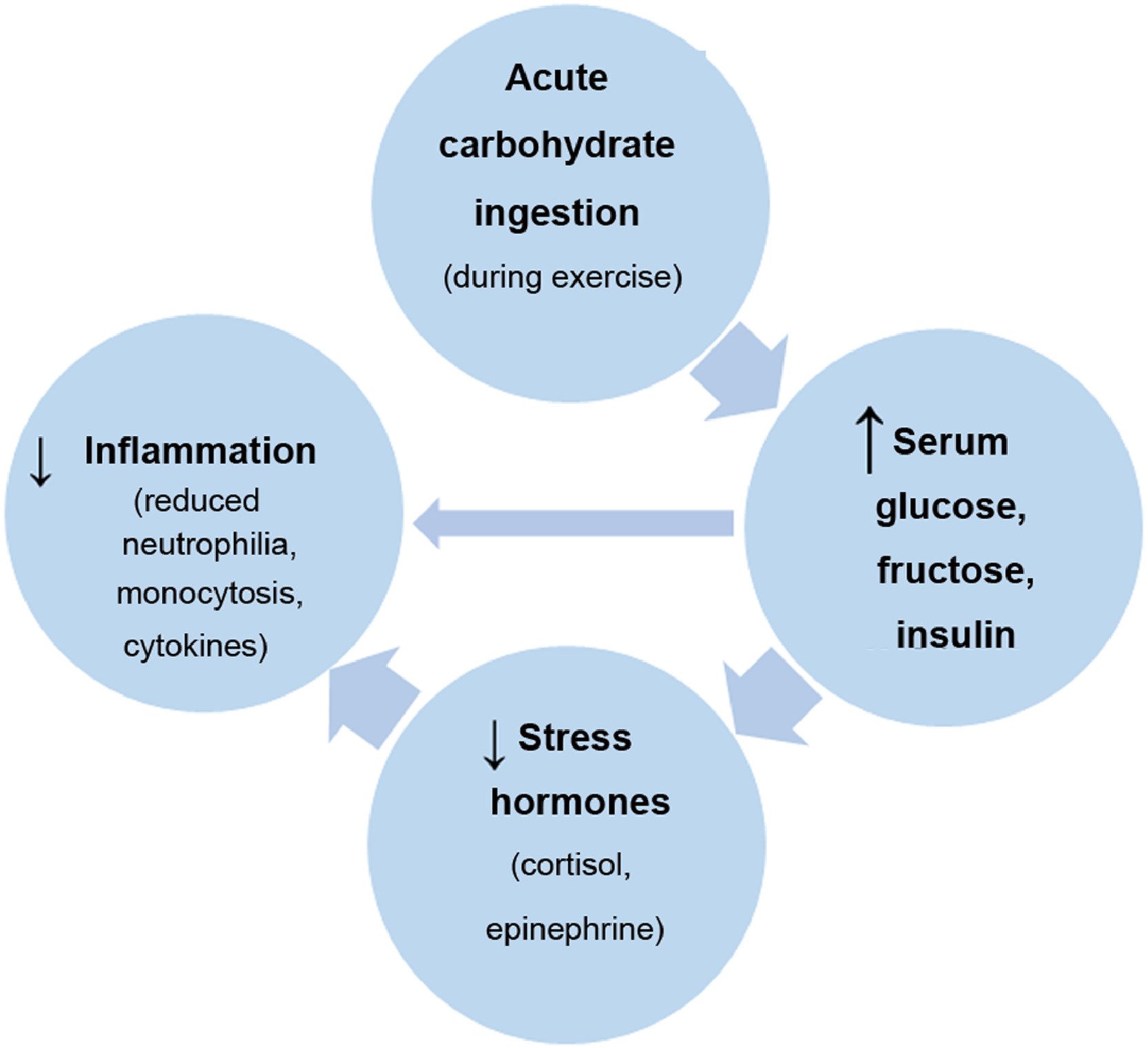
Further studies have found that consuming carbohydrates before and during endurance exercise can help reduce levels of cortisol (a stress hormone), lower inflammation markers, and support a stronger immune response (see Figure 2). This highlights how essential proper nutrition is for athletes looking to maintain a healthy immune system.
Some Science - Immune System
Our immune system is like the body’s Defence team—it protects us from germs, infections, and illnesses. It’s always on the lookout for anything harmful, like viruses or bacteria. There are two main parts to it: one that reacts quickly to any threat (the innate immune system) and one that learns and remembers past threats to fight them better next time (the adaptive immune system).
To work properly, the immune system needs the right fuel, which comes from the food we eat. A healthy diet with plenty of vitamins, minerals, proteins, and healthy fats helps keep it strong and lowers the risk of long-term inflammation. As well as diet, exercise also plays important role in the strength of immune system, stress hormones and inflammation.
The Crucial Role of Nutrition in Immune Function
The immune system’s energy and nutrient needs are met through diet and body stores. Micronutrients, acquired primarily from food, are essential for immune development and function. Nutrients like vitamins A, C, and D, as well as zinc and iron, regulate immune cell functions, enhancing the body's ability to fight infections. A balanced diet supports the immune system through life stages, while undernutrition weakens immune responses and increases vulnerability to infections.
Gut-Associated Lymphoid Tissue (GALT): A Critical Immune Hub
Most immune cells reside in the gut-associated lymphoid tissue (GALT), which performs essential sensing and immune functions. Disruptions like “leaky gut” can lead to inappropriate immune responses. The gut microbiota, composed of trillions of microorganisms, plays a vital role in immune health. Probiotics and prebiotics support a healthy microbiome, which in turn supports immune function. A plant-based diet, rich in diverse nutrients, can enhance microbiota diversity, further boosting both gut and immune health.
Figure 1: Nieman, D.C. and Wentz, L.M. (2019)
Key Nutrients That Support Immune Function
Several nutrients are crucial in maintaining immune system function. A diverse diet, especially one rich in plant-based foods, supports immune health. Here are some key nutrients for immune support:
Vitamin C: This potent antioxidant protects immune cells from oxidative damage and enhances neutrophil, macrophage, and lymphocyte function. It also supports antibody production. Sources include citrus fruits, broccoli, strawberries, and kale.
Vitamin D: Essential for regulating immune responses, vitamin D activates T cells and enhances pathogen-fighting effects of macrophages. A deficiency is linked to increased infection risks and autoimmune diseases. Found in sunlight, egg yolk, and fatty fish.
Zinc: This trace mineral plays a pivotal role in immune cell development and activation. Zinc also protects cells from oxidative stress during immune responses. Sources include nuts, seeds, meat, fish, and whole grains.
Vitamin A: Vital for maintaining epithelial barriers in the skin, respiratory tract, and gut, vitamin A supports immune cell function and acts as the body’s first defense against pathogens. Found in leafy vegetables, carrots, sweet potatoes, and fish oils.
Selenium: Selenium is a powerful antioxidant that protects immune cells from oxidative damage. It supports neutrophils, macrophages, and natural killer cells, which play vital roles in immune defense. Sources include Brazil nuts, eggs, and bananas.
Iron: Iron supports the proliferation of immune cells, particularly lymphocytes. It also helps produce hemoglobin, which transports oxygen to immune tissues. Iron is found in red meat, beans, and spinach.
Omega-3 Fatty Acids: Found in fatty fish, omega-3s reduce excessive inflammation and enhance immune cell function. They are especially important for macrophages and T cells.
Protein: Proteins are necessary for immune cell and antibody synthesis. Amino acids like glutamine and arginine support immune cell proliferation and function.
Carbohydrates & Fibre: Prebiotic fiber feeds beneficial gut bacteria, supporting microbiome health and enhancing immune function. The fermentation of fiber produces short-chain fatty acids, which have anti-inflammatory properties and further support immune responses.
Conclusion
If you are training for marathons it is important to prioritize your rest days, sleep, Hygiene, diet, and psychological stress to reduce risk of illness and infection. Incorporating a diet rich in diverse plant foods, and adding carbohydrates before and During longer or high intensity training sessions is a must.
Reference List
Nieman, D.C. and Wentz, L.M. (2019) ‘The compelling link between physical activity and the body’s defense system’, Journal of Sport and Health Science, 8(3), pp. 201–217. doi:10.1016/j.jshs.2018.09.009.
Childs, C.E., Calder, P.C. and Miles, E.A. (2019) ‘Diet and immune function’, Nutrients, 11(8), p. 1933. doi:10.3390/nu11081933.
Farré, R. et al. (2020) ‘Intestinal permeability, inflammation and the role of nutrients’, Nutrients, 12(4), p. 1185. doi:10.3390/nu12041185.
Figure 2: Nieman, D.C. And Wentz (2019)